Understanding Different Types of Medicine
Medically reviewed by
According to the World Health Organization, health is “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.” (14) Achieving or maintaining good health is a lifelong process that generally involves working with a variety of healthcare providers. There are various types of medical approaches that each provide unique viewpoints and contributions to the field of healthcare.
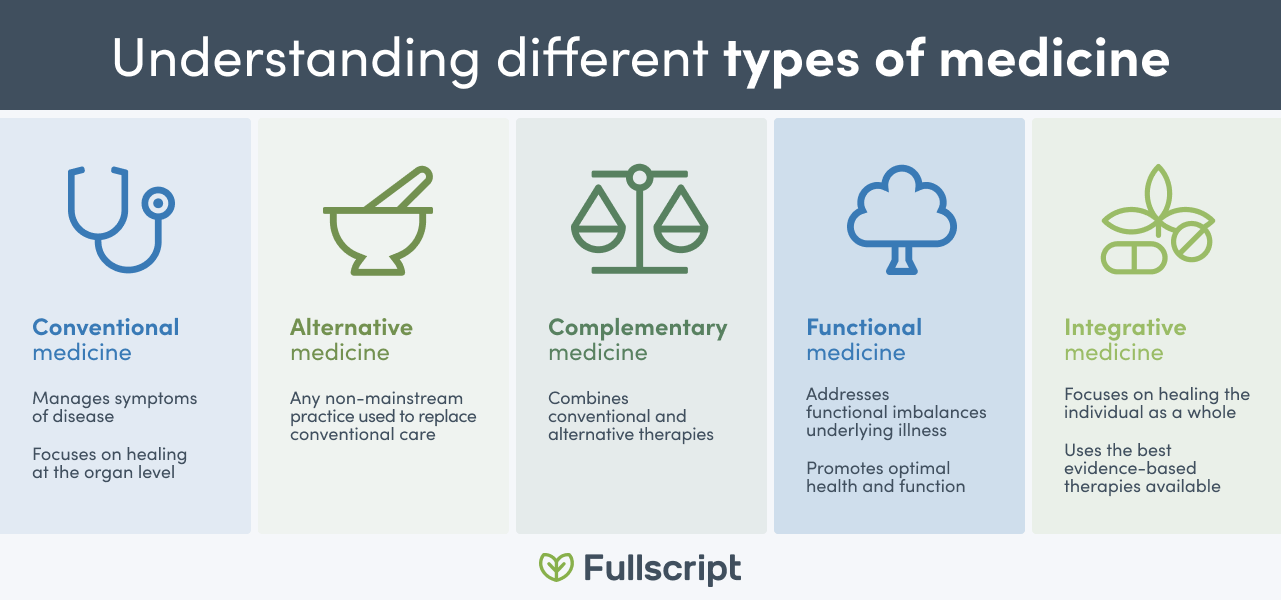
Continue reading to learn about conventional medicine and complementary medical systems, including integrative and functional medicine.
What is conventional medicine?
Conventional medicine also referred to as allopathic, mainstream, and Western medicine, is defined as a system in which healthcare practitioners use approaches, such as pharmaceutical medication, radiation, or surgery to treat symptoms and diseases. Conventional treatments are widely used by many healthcare professionals, including medical doctors, nurses, and pharmacists. (9) Medical literature suggests that while conventional care manages the symptoms of disease, the etiology (underlying cause) is often not considered. (3) This approach is said to focus on treating at the symptom level, rather than the individual as a whole. (4)
Did you know? Over 30 percent of U.S. adults and 12 percent of children use health care approaches outside of the conventional medical model. (10)
Complementary and alternative medicine
In addition to the conventional healthcare model, there are a variety of different medical models collectively referred to as complementary and alternative medicine (CAM). CAM systems differ from conventional medicine as they commonly view and treat dysfunction as an imbalance within the whole person, rather than as distinct issues occurring in a specific body system. (4)
For example, when treating hypertension (elevated blood pressure), a physician practicing conventional medicine may prescribe pharmaceutical medication to lower blood pressure. On the other hand, a functional medicine physician would assess possible inflammation, oxidative stress, and vascular immune dysfunctions involved and address them with lifestyle approaches including the use of antioxidants, exercise, meditation, nutrition, supplements, and weight loss, as well as pharmaceuticals in some instances. (2)
Examples of CAM systems include:
- Ayurveda
- Functional medicine
- Homeopathy
- Naturopathy
- Traditional Chinese medicine (TCM) (10)
A CAM system generally uses several complementary techniques. For example, TCM, as a whole, incorporates acupuncture, botanicals, diet, environmental practices, and qi gong (a traditional Chinese practice of breathing, meditation, and movement) in individualized treatments. (4)
Conventional medicine versus alternative medicine
Alternative medicine is considered to be any non-mainstream practice used to replace conventional care. (10) For instance, when a natural product or special diet is used instead of a pharmaceutical medication to address a health condition, it is known as an alternative treatment. (9)
Complementary medicine
Conventional and alternative medicine don’t necessarily exist exclusively. When a non-mainstream approach is used in combination with conventional medicine, it is known as complementary medicine. (10)
Approaches or techniques used in complementary medicine encompass natural products, manual therapies, and mind-body practices, including:
- Acupuncture
- Chiropractic manipulation
- Supplementation (e.g., botanical herbs, probiotics, vitamins, minerals)
- Meditation
- Qi gong
- Tai chi
- Yoga (10)
Did you know? The number of adults in the U.S. practicing yoga has increased, growing from 9.5 percent in 2012 to over 14 percent in 2017. (10)

Challenges with using CAM
Many CAM systems have faced critique or marginalization as a result of differences between conventional and complementary medicine. Each CAM system has a unique underlying philosophy, with methods of diagnosing and treating individuals that often do not align with conventional methods. (4)
Conventional or Western research and medicine have identified certain concerns with CAM, including:
- Challenges with incorporating methods in conventional practice (4)
- Insufficient evidence
- Issues establishing safety and efficacy of treatments
- Poor training and regulation of practitioners
- Unsubstantiated health claims (13)
The above concerns may, in part, be due to limitations in research, resulting in an incomplete understanding of CAM and its benefits. For example, research may be driven by consumer interest in certain services over others. Additionally, the distinct philosophies and categorization of patients in each CAM system cannot easily be studied using the same scientific methods or outcome criteria as conventional medicine. (4)(8)
Conventional practitioners are faced with several challenges when discussing CAM practices with patients or making lifestyle and nutrition recommendations, (3)(11) which are commonly included in guidelines for managing chronic conditions such as diabetes and cardiovascular disease. These challenges may include the practitioner’s level of knowledge or education in nutrition, their confidence in the scientific evidence available, as well as the limited time they may spend with their patients. (3)

What is functional medicine?
Functional medicine (FM), pioneered by the Institute for Functional Medicine (IFM) in 1991, (5) is a system that addresses underlying symptoms and functional imbalances to reverse illness and promote optimal health and function. FM views biological functions as interconnected, and functional imbalances occurring as a result of interactions between genes and environmental factors, including environmental toxins, lifestyle, microbiome, and social determinants. (3)
A functional approach views these biological functions as factors that are changing, and disease as an endpoint to this process. In this approach, a healthy function is assessed at different levels, including the spiritual, social, body system, organ, tissue, cellular, or subcellular levels. (3)(5)
Functional medicine in practice
The FM practice model may include a functional medicine doctor as a primary care physician, as well as a behavioral therapist, dietician, and health coach as part of a care team. (3) To address the individual’s functional needs, a personalized therapeutic program is developed (5) that may include diet, lifestyle interventions, medication, and dietary supplements. (3)
One study compared the self-reported quality of life in patients receiving care at the Cleveland Clinic Center for Functional Medicine (FM) or a Cleveland Clinic family health center (conventional medicine). The study included 7,252 individuals with a variety of conditions, including depression, diabetes, and hypertension. At both six and 12 months, the study found that greater improvements in quality of life were seen in the FM clinic group compared to the conventional care group. The self-reported quality of life measures included emotional problems, fatigue, mental health, overall quality of life, pain intensity, physical functioning, physical health, and satisfaction with social activities. (3)
The researchers suggest that the greater improvement in quality of life may be due to the long duration of the first FM visit, 60 to 75 minutes, as well as the multidisciplinary care provided by a team of practitioners. In comparison, one study found that primary care visits with a physician practicing conventional medicine are approximately 15 minutes, with individual health topics receiving attention for between one to five minutes of the appointment. (12) Additionally, the FM model involved therapeutic partnerships between the providers and patients, emphasizing open communication, giving patients responsibility for their health, and using empathetic language. (3)
What is integrative medicine?
Medical researchers and clinicians commonly understand Integrative medicine (IM) as combining conventional medicine with complementary and alternative medicine (CAM) approaches. However, this combination does not capture the full scope of integrative medicine and what it has to offer. (4)
The Academic Consortium for Integrative Medicine & Health provides this definition: “Integrative medicine and health reaffirms the importance of the relationship between practitioner and patient, focuses on the whole person, is informed by evidence, and makes use of all appropriate therapeutic and lifestyle approaches, healthcare professionals and disciplines to achieve optimal health and healing.” (1)
IM is an umbrella system that approaches treating the individual as an indivisible whole, including community, emotional, environmental, functional/physical, social, and spiritual domains. (4)(8)(10) Healing is viewed as occurring from within the patient, rather than an action by the practitioner. (4)
The IM system focuses on coordination between various healthcare providers and institutions (10) to empower the patient through therapeutic, supportive relationships between the patient and practitioner. (11) The individual and practitioner work together to develop an integrative treatment plan that incorporates both conventional and alternative techniques that are evidence-based. (4)(8)(11)

Integrative medicine in practice
Scientific literature suggests that IM has been incorporated into clinical practice in various ways. One model combines the medical research and clinical experience behind both conventional and CAM approaches, resulting in a fairly equal partnership between the two. A second model uses only evidence-based aspects of CAM in conventional medicine. (13) IM is practiced to a varying extent at the practitioner, clinic, team, or health system level. (8) The CAM-conventional division can be understood as a scale, with some practitioners or clinics as more CAM-oriented, and others as more oriented toward conventional medicine. (8)
One study examined the model of care at the University of Arizona Integrative Health Center (UAIHC) primary care clinic. integrative medicine doctors at the clinic work alongside a multidisciplinary team including a behavioral health clinician, acupuncturist, chiropractor, dietician, health coach, and nurse who have received additional training in IM. The practice model includes a comprehensive patient health intake, assessing lifestyle factors (e.g., diet, physical activity, relationships, sleep, spirituality, stress), a Health Partnership Agreement between the individual and their provider, a decision-making process involving the individual, as well as groups, classes, and health coaching to support lifestyle changes. The study found that patient surveys reported that the UAIHC successfully provided integrative care (aligned with the IM model) that resulted in high overall patient satisfaction. (6)
IM has also been studied at the Benson-Henry Institute (BHI) for Mind Body Medicine at Massachusetts General Hospital. The clinic uses a comprehensive (mind-body-spirit) program known as the Relaxation Response Resiliency Program (3RP) intended to help individuals manage stress, increase resiliency, and develop coping skills. The program, facilitated by a team of nurses, physicians, psychologists, and social workers, focuses on preventing disease using lifestyle choices, self-care, and empowering techniques. In addition to reduced stress, research has found 3RP to be associated with a reduced number of medical visits and procedures. (7)
The bottom line
Various medical systems and approaches may be used to improve health, each with unique contributions to the field of medicine. Functional and integrative medicine are two systems that view health as a positive quality, rather than only as the absence of disease. (4)(5) When considering different approaches, we encourage you to research and think critically about the type of support you need and desire to maintain your health or achieve specific health goals.
References
- Academic Consortium for Integrative Medicine & Health. (2018). Mission. Retrieved April 21, 2020, from https://imconsortium.org/about/mission/
- Alexander, W. (2014). Hypertension: Is it time to replace drugs with nutrition and nutraceuticals? Pharmacy and Therapeutics, 39(4), 291–295.
- Beidelschies, M., Alejandro-Rodriguez, M., Ji, X., Lapin, B., Hanaway, P., & Rothberg, M. B. (2019). Association of the functional medicine model of care with patient-reported health-related quality-of-life outcomes. JAMA Network Open, 2(10), e1914017.
- Bell, I. R., Caspi, O., Schwartz, G. E., Grant, K. L., Gaudet, T. W., Rychener, D., … Weil, A. (2002). Integrative medicine and systemic outcomes research: Issues in the emergence of a new model for primary health care. Archives of Internal Medicine, 162(2), 133–140.
- Bland, J. (2017). Defining function in the functional medicine model. Integrative Medicine (Encinitas, Calif.), 16(1), 22–25.
- Crocker, R. L., Grizzle, A. J., Hurwitz, J. T., Rehfeld, R. A., Abraham, I., Horwitz, R., … Maizes, V. (2017). Integrative medicine primary care: Assessing the practice model through patients’ experiences. BMC Complementary and Alternative Medicine, 17(1), 490.
- DiLauro, M. D. (2018). Examination of an integrative health care model for social work practice. Health & Social Work, 43(4), 261–268.
- Kania-Richmond, A., & Metcalfe, A. (2017). Integrative health care – What are the relevant health outcomes from a practice perspective? A survey. BMC Complementary and Alternative Medicine, 17(1), 548.
- National Cancer Institute. (n.d.). NCI Dictionary of Cancer Terms. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms
- National Center for Complementary and Integrative Health. (n.d.). Complementary, alternative, or integrative Health: What’s in a name? Retrieved from https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
- Ring, M., & Mahadevan, R. (2017). Introduction to integrative medicine in the primary care setting. Primary Care: Clinics in Office Practice, 44(2), 203–215.
- Tai-Seale, M., McGuire, T. G., & Zhang, W. (2007). Time allocation in primary care office visits. Health Services Research, 42(5), 1871–1894.
- Templeman, K., & Robinson, A. (2011). Integrative medicine models in contemporary primary health care. Complementary Therapies in Medicine, 19(2), 84–92.
- World Health Organization. (n.d.). Constitution. Retrieved from https://www.who.int/about/who-we-are/constitution
